Poker Chip Tool Pain Scale Age
- Vintage & antique measuring scales, 6 inch metal rules, old tool advertising rulers Collection of seven 6' metal rules with some nice old advertising from hardware sellers. These are all in good clean condition overa.
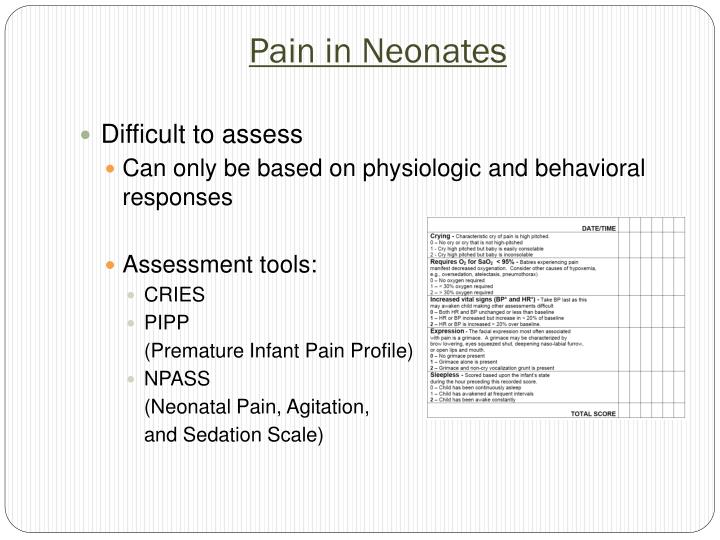
- The poker chip tool has been used with success in children aged 3 to 5 years and its validity has been established by high correlations in pain ratings assigned using the PCT and the Hurt Thermometer as well as the PCT and the Oucher tool. One study however, found that most children, nurses and parents preferred the Faces scale to the PCT.
To create ambiguity, a gray occluder covering 50 of the poker chips is displayed; the subject knows there are at least 25 red and 25 blue chips. The remaining 50 can be any combination of red and blue, implying that the odds of winning $20 can be anywhere from 25% to 75%. 1C presents the three possible ambiguous lotteries.

- Stewart B, Lancaster G, Lawson J, Williams K, Daly J. Validation of the Alder Hey Triage Pain Score. Arch Dis Child. 2004;89(7):625-630.
- Dehghani H, Tavangar H, Ghandehari A. Validity and reliability of behavioral pain scale in patients with low level of consciousness due to head trauma hospitalized in intensive care unit. Arch Trauma Res. 2014;3(1):e18608.
- Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the Brief Pain Inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain. 2004;20(5):309-318.
- Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129-138.
- Feldt KS. The checklist of nonverbal pain indicators (CNPI). Pain Manag Nurs. 2000;1(1):13-21.
- Busner J, Targum S. The Clinical Global Impressions Scale. Psychiatry (Edgmont). 2007;4(7):28-37.
- Boitor M, Fiola JL, Gelinas C. Validation of the critical-care pain observation tool and vital signs in relation to the sensory and affective components of pain during mediastinal tube removal in postoperative cardiac surgery intensive care unit adults. J Cardiovasc Nurs. 2015 Mar 30 [Epub ahead of print].
- Gelinas C, Harel F, Fillion L, Puntillo KA, Johnston CC. Sensitivity and specificity of the critical-care pain observation tool for the detection of pain in intubated adults after cardiac surgery. J Pain Symptom Manage. 2009;37(1):58-67.
- Andersen T, Christensen FB, Bunger C. Evaluation of a Dallas Pain Questionnaire classification in relation to outcome in lumbar spinal fusion. Eur Spine J. 2006;15(11):1671-1685.
- Doctor JN, Slater MA, Atkinson JH. The Descriptor Differential Scale of Pain Intensity: an evaluation of item and scale properties. Pain. 1995;61(2):251-260.
- Gracely R, Kwilosz D. The Descriptor Differential Scale: applying psychophysical principles to clinical pain assessment. Pain. 1988;35(3):279-288.
- Watanabe SM, Nekolaichuk CL, Beaumont C. The Edmonton Symptom Assessment System, a proposed tool for distress screening in cancer patients: development and refinement. Psychooncology. 2012;21(9):977-985.
- Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010;17(1):50-54.
- Douglas ME, Randleman ML, DeLane AM, Palmer GA. Determining pain scale preference in a veteran population experiencing chronic pain. Pain Manag Nurs. 2014;15(3):625-631.
- Melzack R. The McGill Pain Questionnaire. In: Melzack R, ed. Pain Measurement and Assessment. New York, NY: Raven Press; 1983:41-47.
- Wheeler AH, Goolkasian P, Baird AC, Darden BV 2nd. Development of the Neck Pain and Disability Scale. Item analysis, face, and criterion-related validity. Spine. 1999;24(13):1290-1294.
- Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25(24):3115-3124.
- Hearn J, Higginson I. Development and validation of a core outcome measure for palliative care: the palliative care outcome scale. Qual Health Care. 1999;8(4):219-227.
- Ohnhaus EE, Adler R. Methodological problems in the measurement of pain: a comparison between the verbal rating scale and the visual analog scale. Pain. 1975;1(4):379-384.
This material must not be used for commercial purposes, or in any hospital or medical facility. Failure to comply may result in legal action.
Medically reviewed by Drugs.com. Last updated on Nov 16, 2020.
- Care Notes
- Overview
What do I need to know about my child's pain?
Children feel and express pain in different ways. Your child may or may not be able to tell you he is in pain. Something that may be painful to one child may not be painful to other children. Your child's pain may be acute (short-term) or chronic (long-term). Pain management is an important part of your child's care.
How will I know if my child is in pain?
If your child can talk, he may tell you where he hurts and how bad it is. If you have a baby or small child, you may need to watch them for signs of pain. You may notice the following behaviors:
- Restlessness
- High-pitched crying
- Not moving or holding himself in a position to decrease pain
- Pulls away or gets upset when he is touched
- Touches, tugs, or rubs the part of his body that is painful
- Eats less or not at all
- Sleeps more or less than usual
What is a pain scale?
A pain scale is a tool used by your child's caregiver to help measure your child's pain. Your child's caregiver uses the pain scale together with examining your child. Your child's caregiver may use any of the following pain scales:
- Faces pain scale: This scale consists of different faces, from happy (no pain) to sad (a lot of pain). Your child may be asked to point to the face that best shows how he feels.
- Body outline tool: Your child will be asked to mark an X or color the painful area on a drawing of a child's body. Different colors can be used to measure his pain.
- Colored analog scale: This scale assigns colors to mild, moderate, or severe pain. Your child will be asked to point to the color that shows how much pain he is in.
- Oucher scale: This scale is used in children who can count. Your child will be asked to point to a number from 10 to 100 to show the amount of pain he is in.
- Poker chip tool: Your child will be asked to pick the number of poker chips to show the level of his pain. One chip represents a small amount of pain and 4 chips is the most amount of pain.
What medicines are used to control pain?
- Ibuprofen or acetaminophen: These medicines help decrease your child's pain. They can be bought without a doctor's order. Ask how much medicine is safe to give your child and how often to give it.
- Narcotic analgesics: These medicines include codeine and morphine. They are used for moderate to severe pain.
- Patient-controlled analgesia (PCA): This is a device that uses an electric pump to give your child pain medicine through an IV. The IV is placed in your child's vein, usually in his arm. Your child receives medicine by pushing a button. Ask your child's caregiver for more information about PCA.
- Anesthetics: These may be injected in or around a nerve to make your child more comfortable. It works by blocking pain signals from the nerves.
What are the side effects of pain medicines?
- Nausea, vomiting, or constipation
- Itching
- Pain in the lower abdomen or trouble urinating
- Irregular heartbeat or seizures
- Trouble breathing
Why is pain control important?
If pain is not treated, it can decrease your child's appetite and affect how well he sleeps. It may also decrease his energy and ability to do things. Pain may also change your child's mood and relationships with others. If pain is treated, your child will feel better and may heal more quickly.
How can I help manage my child's pain?
- Give your child his pain medicine as directed: Follow instruction on how much and how often to give your child medicine.
- Do not wait until your child's pain is severe: The medicine may not work as well at controlling the pain if you wait too long to give it. Tell your child's caregiver if your child's pain gets worse.
Poker Chip Tool Pain Scale Age Range
When should I contact my child's caregiver?
Contact your child's caregiver if:
- Your child has a fever.
- Your child has nausea or vomiting.
- Your child is more sleepy than usual after he takes his medicine.
- You have questions or concerns about your child's condition or care.
When should I seek immediate care?
Seek care immediately or call 911 if:
- Your child's skin becomes red, swollen, and itchy.
- Your child suddenly has trouble breathing.
- Your child is sad, depressed, or not able to cope with his pain or illness.
- Your child's pain does not get better, or he has new pain.
Care Agreement

You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's caregivers to decide what care you want for your child.
Further information
Poker Chip Tool Pain Scale Age Guide
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.